ANDERS.LASSEN-NIELSEN.COM
|
|
Case studies |
Case list:
|
Reduce redundency in ERUsing a Lean Management approach it was possible
to reduce redundant functions in
the way a healthcare provider handled 'acute' patient. 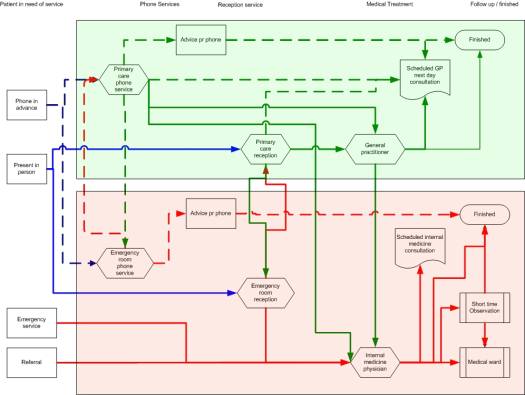
Figure 1 shows the 'acute flow' before reorganized 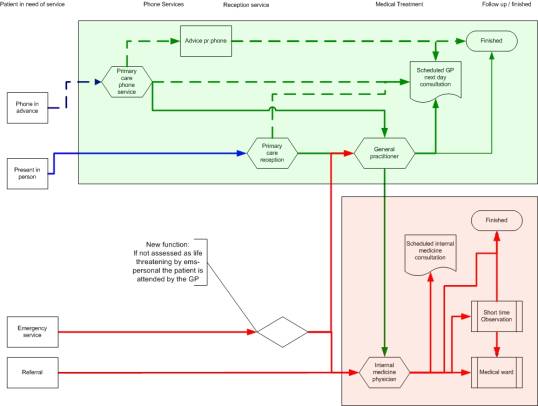
Figure 2 shows the 'acute flow' after it reorganized
Reduce bottlenecks in ERUsing Discrete Event Simulation to identify bottlenecks in an ER and subsequence make a simple rearrangement of staff duties. For more details see my publication A. Lassen Nielsen, H. Hilwig, N. Kissoon, S.
Teelucksingh. Discrete event simulation as a tool in
optimization of a professional complex adaptive system.
Stud Health Technol Inform. 2008;136:247-52
and the presentation from MIE 2008
Figure 1 shows the patient flow in the ER Initially 174 patients were seen on an average 24 hour shift. The average
waiting time was 9.2 hours.
The simulation showed that the 1st Triage nurse had a 99.5%
utilization, the clerk 73.9%, the emergency physician 44.3% and the ECG-nurse only 6.9%. Predicting the need for hemodialysis capacity.Discrete Event Simulation is a logical (or mathematical) model of a system where changes occur at separate points in time. Even though most changes related to RRT happen at separate points some changes occur as a continues process as well, hence a more appropriate term describing our model would be as a mixed continuous-discrete model1. The core of our simulation model is the universal RRT model as originally presented by Davies & Roderick. It basically deals with the flow of patients within what we could call the ‘chronic RRT-core’. It admits patients with ESRD onto RRT based on known gross incidences of patients in need of RRT. The model then simulates interaction between the three available modalities (PD, HD, TX) based on known frequencies on transfer between the modalities. There is by nature only one-way out of the model, namely death. Hence mortality within each of the modalities determines a patient’s exit. The strengths of this model is its simplicity and universality. For example, an intervention resulting in improved survival can be easily entered into the model thereby permitting a mathematical assessment of this intervention. See poster presented at EDTA meeting 2010
See poster presented at 'EVIDENCE 2011' conference London, UK
Curriculum mappingTake a tour of the brain: Starting with the kidney curriculum/syllabus Opens in a new window If it has caught your interest please contact me for more information >Contact
|